Laboratory Test
Anti–acetylcholine receptor antibody
The anti–acetylcholine receptor (AChR) antibody (Ab) test is reliable for diagnosing autoimmune myasthenia gravis (MG). It is highly specific (as high as 100%, according to Padua et al). [4] Results are positive in as many as 90% of patients who have generalized MG but in only 50-70% of those who have only ocular MG; thus false negatives are common in cases of purely ocular MG.
False-positive anti-AChR Ab test results have been reported in cases of thymoma without MG and in patients with Lambert-Eaton myasthenic syndrome, small cell lung cancer, or rheumatoid arthritis treated with penicillamine, as well as in 1-3% of the population older than 70 years.
Tindall reported AChR Ab results and mean Ab titers in a group of patients with MG (see the Table below). [25]
Table. Prevalence and Titers of Antibody to Acetylcholine Receptor in Patients with Myasthenia Gravis (Open Table in a new window)
| Osserman MG Class* | Mean Anti-AChR Titer (× 10–9 M) | Positive Results, % |
| R | 0.79 | 24 |
| I | 2.17 | 55 |
| IIA | 49.8 | 80 |
| IIB | 57.9 | 100 |
| III | 78.5 | 100 |
| IV | 205.3 | 89 |
| AChR = acetylcholine receptor; MG = myasthenia gravis. *Osserman classification: R = remission, I = ocular only, IIA = mild generalized, IIB = moderate generalized, III = acute severe, IV = chronic severe. |
These data suggest a trend toward higher Ab titers in more severe disease, though the titer does not predict severity in an individual patient. Changes in the anti-AChR titer correlate with long-term improvement induced by prednisone or azathioprine; the same changes are not observed consistently in patients who undergo thymectomy. However, this finding is not consistent, and serial Ab titers alone are not reliable. Accordingly, serial Ab titers by themselves are not clinically useful for judging a patient’s response.
Anti–striated muscle antibody
The anti–striated muscle (anti-SM) Ab test is also important in patients with MG. Anti-SM Ab is present in about 84% of patients with thymoma who are younger than 40 years and less often in those without thymoma. Thus, a positive test result should prompt a search for thymoma in patients younger than 40 years. In individuals older than 40 years, anti-SM Ab can be present without thymoma.
Anti-MuSK antibody
About half of the patients with negative results for anti-AChR Ab (seronegative MG) may have positive test results for antibody to muscle-specific kinase (MuSK), a receptor tyrosine kinase that is essential for neuromuscular junction development. [26] These patients may represent a distinct group of autoimmune MG, in that they show some collective characteristics that are different from those of anti-AChR–positive patients. [27]
Anti-MuSK–positive individuals tend to have more pronounced bulbar weakness and may have tongue and facial atrophy. They may have neck, shoulder and respiratory involvement without ocular weakness. They are also less likely to respond to acetylcholine esterase (AChE) inhibitors, and their symptoms may actually worsen with these medications.[28, 29]
Anti-lipoprotein-related protein 4 (LRP4) antibody
Lipoprotein-related protein 4 is present on the postsynaptic membrane and is a receptor for agrin and is essential for neuromuscular junction formation. Antobody to this protein is present in 2-27% of double seronegative myasthenics (absence of AChR and Anti-MuSK antobodies) [30] .
Antistriational antibody
Serum from some patients with MG possesses antibodies that bind in a cross-striational pattern to skeletal and heart muscle tissue sections. These antibodies react with epitopes on the muscle protein titin and ryanodine receptors (RyR).
Almost all patients with thymoma and MG, as well as half of the late-onset MG patients (onset at 50 years or later), manifest a broad striational antibody response. Striational antibodies are rarely found in anti-AChR–negative patients. They can be used as prognostic determinants in MG; as in all subgroups of MG, higher antibody titers are associated with more severe disease. [31] Because of a frequent association with thymoma, the presence of titin/RyR antibodies should arouse a strong suspicion of thymoma in a young patient with MG.
Other laboratory studies
Testing for rheumatoid factor and antinuclear antibodies (ANAs) is indicated to rule out systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA).
Thyroid function tests are indicated to rule out associated Graves disease or hyperthyroidism. This is essential, especially in patients with ocular MG where the concomitant hyperthyroidism is most frequent.
Radiography, CT, and MRI
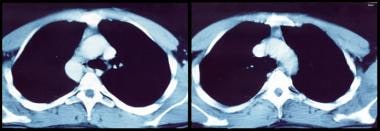
On plain anteroposterior and lateral views, radiography may identify a thymoma as an anterior mediastinal mass. A negative chest radiograph does not rule out a smaller thymoma, in which case a chest computed tomography (CT) scan is required. Chest CT scan should be obtained to identify or rule out thymoma or thymic enlargement in all cases of MG (see the images below). This is especially true in older individuals.
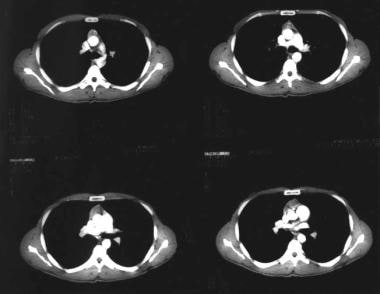 CT scan of chest showing an anterior mediastinal mass (thymoma) in a patient with myasthenia gravis.
CT scan of chest showing an anterior mediastinal mass (thymoma) in a patient with myasthenia gravis.
It is essential to rule out mass lesions compressing the cranial nerves in strictly ocular MG. CT or preferably magnetic resonance imaging (MRI) of the brain and orbit is indicated. It is helpful when the diagnosis of MG is not established and to rule out other causes of cranial nerve deficits. MRI can evaluate for intraorbital or intracranial lesions, basal meningeal pathology, or multiple sclerosis.
Electrodiagnostic Studies
Electrodiagnostic studies can demonstrate a defect of neuromuscular transmission. The following 2 studies are commonly performed:
- Repetitive stimulation of a muscle at 2-3 Hz, also known as repetitive nerve stimulation (RNS)
- Single-fiber electromyography (SFEMG), aimed at evaluating neuromuscular block, jitter, and fiber density
SFEMG is more sensitive than RNS in assessing MG. However, SFEMG is technically more difficult and much more dependent on the experience and skill of the testing physician. Consequently, RNS is the most frequently performed neurophysiologic test of neuromuscular transmission.
Repetitive nerve stimulation
During low-frequency (1-5 Hz) RNS, the locally available acetylcholine (ACh) becomes depleted at all neuromuscular junctions (NMJs), and less is therefore available for immediate release. This results in smaller excitatory postsynaptic potentials (EPSPs).
In patients without MG, all EPSPs exceed the threshold to generate an action potential (ie, there is a safety factor). No change in the summated compound muscle action potential (CMAP) is noted. In patients with MG, the number of AChRs is reduced, lowering the safety factor. During RNS, some EPSPs may not reach threshold, which means that no action potential is generated. This results in the decrement in the amplitude of the CMAP.
In patients with myasthenia gravis, this decremental response usually has a maximum decrement at the fourth or fifth response, followed by a tendency toward repair (see the image below). A stimulation rate of 1-5 per second should result in a 10% or more decrease in amplitude by the fourth or fifth action potential; any decrement over 10% is considered abnormal. The most common employed stimulation rate is 3 Hz.
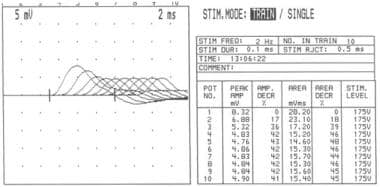 Repetitive nerve stimulation at frequency of 2 Hz showing increasing decrement in amplitude of compound muscle action potential up to fourth response (42% amplitude loss), after which it stabilizes.
Repetitive nerve stimulation at frequency of 2 Hz showing increasing decrement in amplitude of compound muscle action potential up to fourth response (42% amplitude loss), after which it stabilizes.
Patients with MG rarely have a decreased response in a clinically normal muscle. Thus, testing a proximal weak muscle gives a better yield than testing a unaffected distal muscle, even if the latter is technically easier. Testing a facial muscle (eg, the orbicularis oculi) is useful because most patients suffer from eyelid weakness or ptosis. RNS results are less likely to be positive in patients with ocular MG.
Factors affecting results
Several factors can affect RNS results. Lower temperatures increase the amplitude of the CMAPs. Patients with MG may report clinically significant improvement in cold temperatures, and they typically report worsening of ptosis in bright sunlight or on a warm day. Therefore, maintaining a constant and perhaps higher-than-ambient temperature during RNS testing is important to bring out abnormalities of NMJ function. The temperature of the skin overlying the tested muscle should be at least 34°C.
Administration of AChE inhibitors before testing may mask the abnormality and consequently should be avoided for at least 1 day beforehand (even longer for long-acting agents).
Factors related to tetanic contraction may also affect RNS findings. A tetanic contraction of muscle is followed by 2 distinct phases:
- Posttetanic potentiation, occurring for the first 2 minutes after tetanic contraction
- Posttetanic exhaustion, lasting an additional 15 minutes after posttetanic potentiation
During posttetanic potentiation, accumulation of calcium inside the terminal axon causes enhanced mobilization and release of ACh, which overcomes the reduced number of AChRs at the NMJ and thus leads to larger EPSPs with additional recruitment of muscle fibers, resulting in a larger CMAP. In MG, this potentiation may normalize RNS results.
In the posttetanic exhaustion phase, the NMJ is less excitable, and even fewer EPSPs reach threshold. Thus, some patients with an equivocal abnormality on RNS during the resting phase may show clear-cut abnormalities during the posttetanic exhaustion phase.
Tetanic contraction of the muscle can be achieved by applying electrical stimulation to the nerve at a rate of 50 per second for 20-30 seconds. However, this is painful. Voluntary contraction of the muscle for 10 seconds at the maximum force can achieve the same goal without discomfort and is preferred.
Single-fiber electromyography
A concentric needle electrode and other monopolar and bipolar needle electrodes can record single motor unit potentials, but they cannot discriminate individual muscle fibers within the motor unit. The single-fiber needle used in SFEMG, which has a small recording surface, allows recording from individual muscle fibers.
SFEMG is capable of determining jitter (ie, variability of the time interval between the action potentials of 2 single muscle fibers in the same motor unit) and fiber density (ie, number of single-fiber action potentials within recording radius of the needle). Increased jitter (with or without impulse blocking) and normal fiber density are suggestive of a neuromuscular fiber transmission defect (see the image below).
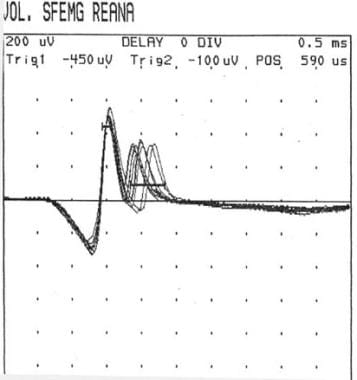 Single-fiber electromyography showing so-called jitter phenomenon (second action potential wave group).
Single-fiber electromyography showing so-called jitter phenomenon (second action potential wave group).
Examination of a weak muscle with SFEMG is more useful than examination with RNS in demonstrating abnormal neuromuscular transmission. SFEMG of the extensor digiti communis (EDC) yields abnormal results in 87% of patients with generalized MG. Examination of a second muscle raises the sensitivity to 99%. In ocular MG, examination of the frontalis is more useful than examination of the EDC. Frontalis findings are abnormal in almost 100% of patients, but only about 60% of EDC findings are abnormal.
Treatment with AChR inhibitors does not normalize SFEMG results. SFEMG findings are abnormal in almost 100% of patients, whereas RNS findings are abnormal in only 44-65%. SFEMG is a good substitute for RNS in patients with ocular MG; a study by Padua et al on 86 patients with ocular MG showed 100% sensitivity. [4] However, SFEMG is technically demanding and highly operator-dependent. In addition, it has a lower specificity, and it can give positive results in other neuromuscular disorders.
Anticholinesterase Test
In patients with MG, the number of AChRs at the NMJ is low, which results in a decreased number of interactions between ACh and its receptor. ACh released from motor nerve terminals is metabolized by AChE. As a result, pharmacologic inhibition of AChE increases ACh concentration at the NMJ, improving the chance for interactions between ACh and its receptor. Edrophonium is a short-acting AChE inhibitor that improves muscle weakness in patients with MG.
This test evaluates weakness (eg, ptosis, partial or complete ophthalmoplegia, and forced hand grip) in an involved group of muscles before and after intravenous (IV) administration of edrophonium. Blinding of both the examiner and the patient increases the validity of the test.
To perform the test, a test dose of 0.1 mL of 10 mg/mL edrophonium solution is administered. If no response and no untoward effects are noted, remainder of the drug (0.9 mL) is injected. Sinus bradycardia due to excessive cholinergic stimulation of the heart is a serious complication; consequently, an ampule of atropine should be available at the bedside or in the clinic room while the test is performed.
This test may give both false-negative results and false-positive results. It has a low sensitivity in ocular MG; 50% of patients presenting with eye symptoms will be missed. On the other hand, diseases other than MG, such as amyotrophic lateral sclerosis (ALS) and cavernous sinus lesions can score positive on the test. [32] This test has been combined with electromyography (EMG) and ocular tonography to increase its sensitivity in ocular MG; however, it still produces false-negative and false-positive results.
Edrophonium is being used in combination with the Lancaster red-green screen testing for diplopia. Most patients would show an improvement in some fields of gaze and a worsening in other directions of gaze. Other patients would not appreciate any change.
Ice Pack Test
The ice pack test (ie, placing ice over the lid) has gained interest among ophthalmologists for assessing improvement in ptosis and diplopia in ocular MG. The rationale behind this test is that cooling might improve neuromuscular transmission.
Movaghar and Slavin questioned the validity of such a test by demonstrating that patients with ocular MG actually improve on the ice, heat, and modified sleep tests. [35] Hence, rest might be the cause of the improvement in ocular signs. Both the ice test and the rest test are sensitive and specific in ocular MG.[36]
Histologic Findings
Studies of muscle biopsy specimens showed that the NMJs of patients with MG had only one third as many AChRs as average normal individuals. Morphologic changes, such as simplification of the pattern of postsynaptic membrane folding and an increase in the gap between the nerve terminal and the postsynaptic muscle membrane, also are present.
Lymphofollicular hyperplasia of thymic medulla occurs in 65% of patients with MG and thymoma occurs in 15%.
Comments
Post a Comment